Menstruation is a natural and essential part of a woman’s reproductive health. However, for many women, it can become a challenging experience due to excessively heavy or prolonged bleeding—a condition medically known as menorrhagia. While an occasional heavy period might not be a cause for concern, consistently heavy flow that disrupts your daily life is not something to overlook. Menorrhagia is more common than many realise and often goes undiagnosed, simply because women are told to “deal with it.” But the truth is, help is available, and treatment can significantly improve your quality of life.
What Is Menorrhagia?
Menorrhagia refers to abnormally heavy or extended menstrual bleeding. It is more than just a “heavy flow”—it’s bleeding that’s intense enough to interfere with your physical, emotional, and social well-being.
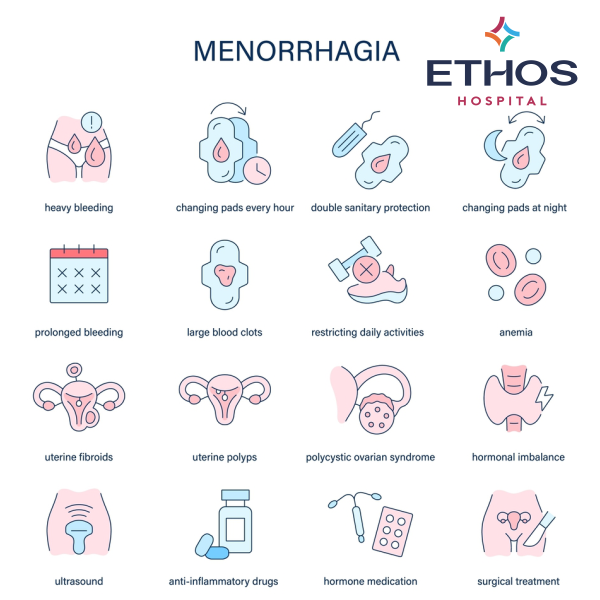
You may be experiencing menorrhagia if you:
- Soak through one or more sanitary pads or tampons every hour for several consecutive hours
- Need to double up on protection (pad + tampon) to avoid leaks
- Wake up at night to change sanitary products
- Experience menstrual periods that last more than seven days
- Pass blood clots larger than a ₹1 coin (or a quarter-sized clot)
- Feel unusually tired, breathless, or weak during your periods—signs of iron-deficiency anaemia due to blood loss
Heavy menstrual bleeding can lead to more than just physical inconvenience. It can cause fatigue, social withdrawal, missed work or school days, and emotional distress. If you find your periods controlling your life, it’s time to explore the cause.
What Causes Menorrhagia?
There are several possible causes of heavy periods. Sometimes, no specific reason is identified. However, some common causes include:
- Hormonal Imbalances: When oestrogen and progesterone levels are out of sync, the uterine lining may thicken more than usual and shed in heavier amounts. This is common in adolescents, women approaching menopause, or those with conditions like polycystic ovary syndrome (PCOS).
- Uterine Fibroids: These non-cancerous growths in the uterus can lead to heavy and prolonged periods, especially in women in their 30s and 40s.
- Polyps: Small, benign growths on the uterine lining may cause irregular or heavy bleeding.
- Adenomyosis: This condition occurs when the tissue that normally lines the uterus grows into the muscular wall, leading to painful and heavy periods.
- Bleeding Disorders: Conditions like von Willebrand disease can prevent proper blood clotting and result in prolonged bleeding.
- Thyroid Disorders: Both hypothyroidism and hyperthyroidism can interfere with normal menstrual patterns.
- Medications: Certain drugs, including anticoagulants (blood thinners), hormonal treatments, and anti-inflammatory medicines, may contribute to heavier bleeding.
- Pelvic Infections or Pregnancy Complications: Infections like pelvic inflammatory disease (PID), or complications such as miscarriage or ectopic pregnancy, can also cause abnormal bleeding.
- Cancer (Rare): In rare cases, cancers of the uterus, cervix, or ovaries may present as heavy or irregular periods, especially in postmenopausal women.

How Is Menorrhagia Diagnosed?
If you suspect that your periods are unusually heavy, it’s important to consult a gynaecologist. Diagnosis typically begins with a thorough medical history and physical examination. Your doctor may ask you to track your menstrual cycle, noting how many pads or tampons you use and any symptoms like fatigue or pain.
Diagnostic tests may include:
- Blood Tests: To check for anaemia or clotting disorders
- Hormone Testing: To identify any hormonal imbalances
- Pelvic Ultrasound: To look for fibroids, polyps, or other structural abnormalities
- Endometrial Biopsy: A sample of the uterine lining is taken for examination, especially if there’s a concern about cancer
- Hysteroscopy: A small camera is inserted into the uterus to detect abnormalities

Treatment Options for Menorrhagia
Treatment depends on the underlying cause, severity of symptoms, age, overall health, and whether or not you wish to have children in the future. Options generally fall into two categories: medical and surgical.
Medical Treatments
- Iron Supplements: Used to treat or prevent anaemia caused by heavy bleeding.
- Non-hormonal medications: Such as tranexamic acid, which helps reduce bleeding during periods.
- NSAIDs or (Non-Steroidal Anti-Inflammatory Drugs): These medications are commonly used to reduce pain, inflammation, and fever. In the context of menorrhagia (heavy periods), NSAIDs like ibuprofen or mefenamic acid can also help reduce menstrual blood loss by decreasing the production of prostaglandins, which are involved in uterine contractions and bleeding.
- Hormonal therapies: Including oral contraceptives, progestins, or a hormonal IUD (like the Mirena), which can thin the uterine lining and reduce bleeding over time.
Surgical Treatments
- Dilation and Curettage (D&C): The uterine lining is scraped to control heavy bleeding or to obtain samples for testing.
- Endometrial Ablation: Destroys the uterine lining and may significantly reduce or stop bleeding—suitable for women who do not plan to become pregnant.
- Myomectomy: Surgical removal of fibroids while preserving the uterus.
- Hysterectomy: Complete removal of the uterus, typically considered a last resort if other treatments are ineffective and future pregnancy is not desired.

When to Seek Help
Heavy periods are not something you should have to simply “put up with.” If your menstrual bleeding interferes with your daily activities, leads to anaemia, or affects your mental well-being, it’s time to speak with a healthcare professional. Early diagnosis and appropriate treatment can greatly enhance your physical health and emotional resilience.
Final Thoughts
Menorrhagia is treatable. With the right combination of medical support and lifestyle management, most women find significant relief and regain control over their menstrual health. You don’t have to suffer in silence—empower yourself with knowledge, advocate for your well-being, and take the first step toward lighter, healthier periods.




